Interesting Science Videos
What is Candida parapsilosis?
Candida parapsilosis has been classified under the emerging pathogens in the recent past, causing invasive candidal disease.
- It was first discovered in Puerto Rico by Ashford in 1928 from a diarrheal stool and later discovered to be a pathogenic agent in causing sepsis among intravenous drug users.
- It was initially named Monilia parapsilosis and later renamed to Candida parapsilosis.
- It is a yeast, that is known to cause sepsis, wound, and tissue infections in immunosuppressed patients, especially neonates and patients in the intensive care units.
- Candida parapsilosis is associated with hyperalimentation (artificial feeding)solutions, prosthetic devices, and indwelling devices, and spread between health care workers and hospitalized patients, through the hands.
- Its virulence has been linked to the secretion of hydrolytic enzymes, the presence of adhesins, and the formation of biofilm.
Habitat of Candida parapsilosis
- Candida parapsilosis is typically a commensal of human skin, and its pathogenicity is limited by the intact integument.
- C. parapsilosis has the ability to grow in total parenteral nutrition (invasive feeding of food to patients) and formation of biofilms on catheters and other implanted devices, for nosocomial spread by hand carriage, and for persistence in the hospital environment.
- The growth of C. parapsilosis is also predominant in nonhuman objects like animals, insects, soil, and marine environments.
- It is also a normal microflora in humans found in the gastrointestinal and respiratory tract and even on the hands.
Morphology of Candida parapsilosis
- Candida parapsilosis cells have an oval, round, or cylindrical shape.
- These cells exist in multiple morphogenetic forms.
- C. parapsilosis does not form true hyphae and exists in either a yeast phase or a pseudohyphal form.
- The morphological forms yeast and pseudohyphae formation have been linked to the production of certain amino acids, citrulline, which makes the cellular and colony morphological changes.
- On medium, the colonies for yeast are smooth while the pseudohyphal colonies are crepe of concentric.
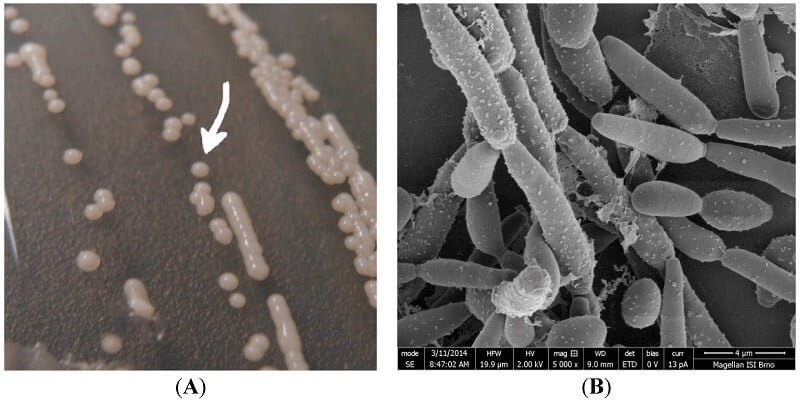
Figure: (A) Image of Candida parapsilosis colonies cultivated on agar for 48 h. The colony size is about 2 mm; (B) SEM (Scanning electron microscopy) image of C. parapsilosis (cultivation for 48 h on a glass substrate), the detailed image was obtained using combined preparation of the two techniques—chemical fixation and freeze-drying (using ACE600 Leica microsystems). Image Source: MDPI.
Cultural characteristics of Candida parapsilosis
- Sabouraud dextrose agar Candida parapsilosis produces white, creamy, shiny, and smooth or wrinkled colonies.
- Cornmeal agar is used to identify Candida parapsilosis pseudohyphae.

Figure: Candida parapsilosis– Pink colored colonies on Hicrome agar. Image Source: Researchgate.
Pathogenesis of Candida parapsilosis
- Candida parapsilosis exists in either a yeast form or a pseudohyphal form. This gives it the advantage to thrive in a wide range of environments
- C. parapsilosis also thrives in medium with high glucose levels, and therefore it will grow rapidly in parenteral nutrition or hyperalimentation solutions feed to patients, which tend to have high concentrations of glucose.
- These factors contribute highly to the risks, transmission, and virulence of the fungi in causing disease on the human host.
Risk factors of Candida parapsilosis infections
- Immunocompromised systems especially HIV/AIDS patients, gastrointestinal surgery patients
- Prolonged use of a central venous catheter or indwelling device, such as cancer patients
- Neonates under hyperalimentation solutions
- Organ transplant patients
- Diabetic patients
- Surgery patients
Transmission of Candida parapsilosis
The transmission of Candida parapsilosis, a yeast fungus that causes invasive fungal infections in majorly transmitted nosocomially from various routes, including:
- Contaminated medical devices
- Contaminated fluids (hyperalimentation solutions)
- Contaminated hands of healthcare workers
- Prosthetic devices
- Invasive catheters
Virulence factors of Candida parapsilosis
Adherence
- This fungus can adhere to indwelling medical devices, which allows the formation of a biofilm that promotes host cell damage.
- The fungus which has a hydrophobicity characteristic contributes to adherence to the surfaces of devices and the formation of a slime that adheres to plastic catheters.
Biofilm formation
- A biofilm is a group of micro-organisms that form on the surfaces of extracellular matrixes. It is a mode of microbial growth on surfaces.
- Candida parapsilosis forms biofilms made up of filaments of pseudohyphae, which adhere to the surfaces of medical devices.
- During biofilm formation, the fungi are able to change in morphology facilitating growth and spread in the medical devices.
- Biofilm formation can also occur on the skin or membrane surfaces, which during device insertion, the fungi gain entry into the device.
- Additionally, biofilms can form on body tissues enhancing the disease spread.
- Biofilm formation also contributes to the fungi resistance to antifungals.
Secretion of hydrolytic enzymes
- Candida parapsilosis produces aspartic proteinases, (Saps), phospholipases, and lipases.
- These hydrolytic enzymes have been linked to the fungi pathogenesis
Clinical Features of Candida parapsilosis
Fungemia
- This is the infection of Candida parapsilosis into the bloodstream, a condition commonly knowns as candidemia.
- It affects hospitalized patients, who have had surgeries especially gastrointestinal surgery patients, making abrasions that allow entry of the commensal Candida into the bloodstream.
- It also affects patients with underlying diseases such as cancer, transplantation, diabetes.
- It is also a common causative agent of candidemia in neonates, patients with intravenous lines or vascular catheters with a previous history of antifungal treatment, patients under parenteral.
- Candida parapsilosis accounts for 19% of all candidemia infections.
- The infection is characterized by fever, septic shock, and renal failure.
Fungal endocarditis
- Candida parapsilosis accounts for 17% of fungal endocarditis infection in heart surgery patients.
- The general predisposing factors for Candida spp being the use of transesophageal ultrasound, and increased use of medical therapies.
- The specific predisposing factors for Candida parapsilosis include prosthetic valves, intravenous drug use, intravenous parenteral nutrition, abdominal surgery, immunosuppression, treatment with broad-spectrum antibiotics, and previous valvular disease, according to research.
- Endocarditis occurs majorly as a result of fungemia, due to tissue infection.
- It affects the aortic valves, mitral valves, tricuspid valves, ventricular wall, and pulmonary valves.
Meningitis
- Common candidal meningitis is associated with symptoms such as headache, photophobia, nuchal rigidity, fever, and delirium.
- Candida parapsilosis causes acute neutropenic meningitis.
- It is transmitted with hospital settings and mostly affects neonates using hyperalimentation solutions and prolonged hospital stay patients, such as transplantation patients.
- It is a progressive infection that occurs due to invasive candidiasis.
- However, the cases are few and rare.
Peritonitis
- It is common in patients with the end-stage renal disease treated with continuous ambulatory peritoneal dialysis.
- the major predisposing factor being long administration on bacterial antibiotics, which facilities the growth and overgrowth of fungi.
- Peritonitis caused by Candida parapsilosis is associated with increasing numbers of polymorphonuclear cells in the blood, abdominal pain, fever, formation of abscesses, and bowel obstruction.
- Evidence from research indicates that Candida parapsilosis is the most common cause of fungal peritonitis.
Ocular infection
- C. parapsilosis causes invasive ocular diseases such as endophthalmitis after surgical operation, and keratitis.
- Endogenous fungal endophthalmitis is rare but not uncommon.
- C. parapsilosis causes keratitis, associated with redness, photophobia, pain, decreased vision, and a yellow-white infiltrate with dry raised slough and feathery edges, and severe disease results in wet, necrotic stromal inflammation similar to another microbial keratitis.
Arthritis
- Fungal arthritis caused by Candida parapsilosis is rare but not uncommon.
- It affects immune-compromised persons (HIV/AIDS), the elderly after arthrocentesis, those receiving joint injections, and patients with implantation of prostheses.
- It can also affect transplant patients.
- It is associated with swelling, tenderness, and decreased movement of the knees.
Vulvovaginitis
- Candida parapsilosis is an uncommon causative agent of vulvovaginitis owing to the fact that Candida albicans causes 99% of these infections in women.
- the 1% is attributed to other candidal agents including C. parapsilosis with is a commensal in the genitourinary tract.
- It is common in pregnant women, diabetic patients, long- administration of antibacterial drugs,
- It is associated with redness, itching, painful urination, burning, dyspareunia, white discharge with an odor.
Otomycosis
- This is a Candida parapsilosis infection of otitis and inflammation of the middle ear or outer ear.
- It is associated with persistent white or colorless otorrhea with tympanum perforation; edema and erythema of tympanic membrane residuum; ear pain; increasing hearing loss; and whitish, cotton-like, or greasy debris in the external auditory canal, tympanic membrane, or residual space due to excision of cholesteatoma.
- It commonly affects immunocompetent patients with chronic hyperplastic inflammation, predisposing them to pathogenic fungi, such as Candida parapsilosis.
- The infection causes an increase in the production of mucus and buildup, which allows fungal colonization.
- Otomycosis has also been linked to the aggressive use of antifungal and antibacterial therapies, predisposing individuals to pathogenic Candida parapsilosis.
Onychomycosis
- This is a common nail infection caused by fungi, but majorly by Candida parapsilosis.
- It is common in elderly persons above the age of 50 years with a thickened nail plate and reduced nail growth, predisposing them to fungal infections.
- It can also affect neonates.
- The predisposing factors include previous traumatic dystrophy of the nail and exposure to the soil during gardening.
- The infection is associated with total dystrophic onychomycosis in chronic mucocutaneous candidiasis, nail dystrophy, hyperkeratosis of nail plates, grooving of the nail ridges, a discolorization of nail margins, onycholysis.
Urinary Tract Infection
- Candida parapsilosis is uncommon in causing UTIs, unlike Candida albicans which causes most of the fungal UTIs.
- However, the 1% is attributed to UTIs of C. parapsilosis and other Candida spp.
- It is associated with asymptomatic infections in women.
Lab Diagnosis of Candida parapsilosis
Specimen: Scrapings (nails), urine, tissue biopsies, centrifuged spinal fluid, blood
Microscopic Examination
- 10% KOH wet mount and calcofluor stains for observation of fungal pseudohyphae under a microscope.
Cultural examination
- Use of SDA medium to observe white, creamy, shiny, and smooth or wrinkled colonies, with tiny blastospores on a mycelial stalk
- Cornmeal Agar used majorly for observing the formation of pseudohyphae.
- Potato Dextrose Agar also white, creamy, shiny, and smooth or wrinkled colonies with larger blastospores.
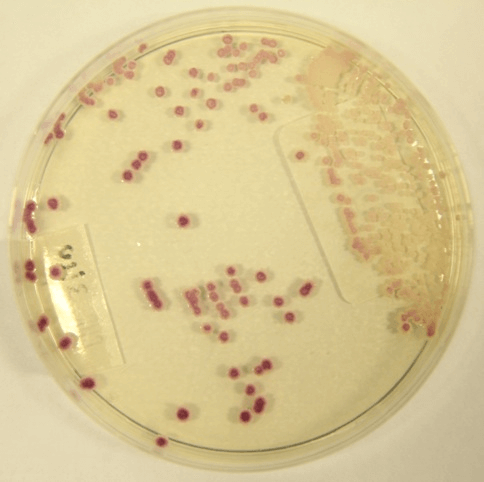
Figure: Candida parapsilosis on CHROMAgar™. Image Source: Leading International Fungal Infection (LIFE).

Figure: Colonies of Candida parapsilosis and C .albicans on Chromogenic candida agar (Biolife). Cultivation 48 hours at 37°C + additional
24 hours at room temperature. Image Source: microbiologyinpictures.com
Biochemical characterization
- For detection of urease production and secretion of hydrolyzing enzymes such as phospholipases.
Molecular Assays
- PCR for identification and detection of the fungal genome.
- Genomic sequencing to distinguish between various candidal groups from samples.
Treatment of Candida parapsilosis infections
- Fungal endocarditis can be treated with Amphotericin B and recurrent endocarditis can use a combination therapy of Amphotericin B and fluconazole (low dosage). Surgical interventions are also recommended.
- Fungal peritonitis can be reduced by the removal of catheters which increase biofilm formation, with intensive combined antifungal therapies of fluconazole, amphotericin B.
- Arthritis caused by C. parapsilosis can be treated with systemic and local administration of amphotericin B, oral flucytosine, and fluconazole. Subsequent doses of fluconazole and flucytosine administered both orally and intravenously for a long period of time; combine therapy of amphoteric B and ketoconazole has also shown some effectiveness;
- C. parapsilosis endophthalmitis can be treated by extracting cataracts, the use of corticosteroid eye drops, intraocular lens implantation, and administration of topical and subtenonian steroids; intraocular and topical amphotericin B can be used for endogenous fungal endophthalmitis and recurrent endophthalmitis.
- Otomycosis can be treated by hygienic washing of the ears followed by the use of topical clotrimazole.
- Urinary tract infections and vulvovaginitis has effectively responded to fluconazole, buconazole, miconazole, or boric acid.
- Other antifungal treatments include echinocandins are the newest class of antifungal agents, which include caspofungin, micafungin, and anidulafungin. These drugs interfere with cell wall synthesis by inhibiting (1, 3)-β-d-glucan synthase, an enzyme that forms glucan polymers, the major component of the fungal cell wall. Caspofungin has potent antifungal activities and less toxin that amphotericin B.
Prevention and control of Candida parapsilosis
- Proper sanitation of intravenous devices for hospitalized patients.
- Removal of catheters to reduce risks of infection
- Proper hygienic hand washing of health care workers when administering to patients to prevent transmission.
References and Sources
- 3% – https://cmr.asm.org/content/21/4/606
- 1% – https://www.thefreelibrary.com/Native+valve+endocarditis+due+to+Candida+parapsilosis+in+an+adult…-a0348569276
- 1% – https://www.sciencedirect.com/topics/medicine-and-dentistry/fungal-endophthalmitis
- 1% – https://www.sciencedirect.com/science/article/pii/S2211505616300072
- 1% – https://www.sciencedirect.com/science/article/pii/S0738081X09002454
- 1% – https://knowthecause.com/echinocandins-a-new-class-of-antifungal-drugs/
- 1% – https://en.wikipedia.org/wiki/Candida_parapsilosis
- 1% – https://cmr.asm.org/content/cmr/21/4/606.full.pdf
- 1% – https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-019-4255-1
- <1% – https://www.uptodate.com/contents/management-of-candidemia-and-invasive-candidiasis-in-adults
- <1% – https://www.thecandidadiet.com/an-introduction-to-candida/
- <1% – https://www.symptoma.com/en/info/candida-meningitis
- <1% – https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/fluconazole
- <1% – https://www.sciencedirect.com/science/article/pii/S0272638612702822
- <1% – https://www.researchgate.net/publication/7705837_Vaginal_Candida_parapsilosis_Pathogen_or_Bystander
- <1% – https://www.nhs.uk/conditions/endocarditis/causes/
- <1% – https://www.ncbi.nlm.nih.gov/pubmed/21570908
- <1% – https://www.ncbi.nlm.nih.gov/pubmed/18854483
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6309157/
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3103236/
- <1% – https://stke.sciencemag.org/content/2006/320/tw40
- <1% – https://microgendx.com/wp-content/uploads/2019/12/The-presence-of-biofilm-structures-in-atherosclerotic-plaques-of-arteries-from-legs-amputated-as-a-complication-of-diabetic-foot-ulcers.pdf
- <1% – https://courses.lumenlearning.com/microbiology/chapter/fungi/
- <1% – https://courses.lumenlearning.com/boundless-biology/chapter/characteristics-of-fungi/
