Interesting Science Videos
What is Campylobacteriosis?
- Campylobacter infection causes human gastroenteritis and vibriosis affecting people worldwide.
- It is a common bacterial disease that usually occurs in both developed and developing countries.
- The disease is endemic in North America, Europe, Australia, Africa, Asia, and the Middle East especially during the summer and early autumn.
- Campylobacteriosis is a food-borne disease that affects children, elders and weakened immune patients mainly in low-income countries however, adults are rarely infected which may be due to their acquired immunity with increasing age.
- Poultry is known to be the main source of Campylobacter infection and they are also present in the GI tract of many wild and farm animals and birds.
- Campylobacter not only causes diarrhea but also causes extragastrointestinal infections such as lung infections, bacteremia, meningitis and long-term autoimmune diseases such as Guillain-Barre syndrome (GBS), Miller-Fisher syndrome (MFS), inflammatory bowel syndrome (IBS) and reactive arthritis (ReA).
- Campylobacteriosis-causing pathogenic species are namely C. jejuni, C. coli, C. upsaliensis, C. lari, C. concisus, C. fetus C. curvas and C. ureolyticus.
- Among them, C. jejuni is associated with 95% of the outbreaks and sporadic illnesses.
- The prevalence of Campylobacter disease is globally therefore; its biocontrol methods, transmission route and prevention are of high concern.
What is Campylobacter?
- Gram-negative
- Non-spore-forming
- Curved, spiral helical or S-shaped rod
- Mostly microaerophilic requires oxygen (3 to 5%) and carbon dioxide (3 to 10%)
- Motility in a corkscrew-like motion
- Grows in temperature 37 to 42°C
- pH 5.5 to 8
- Utilize amino acids for energy
- Sensitive to heat and desiccation (cannot grow above 48°C)
Sources of transmission of Campylobacter
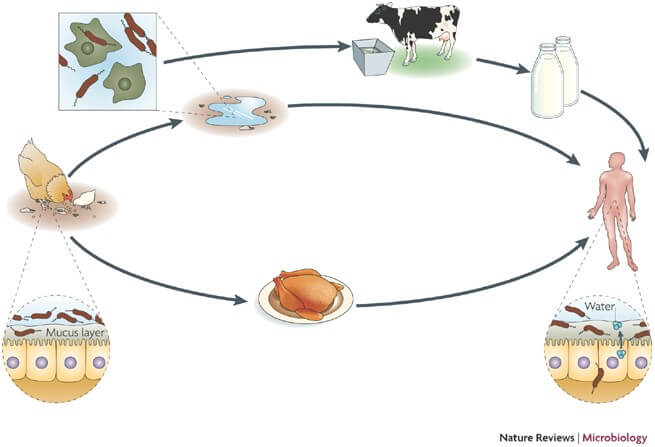
- The main reservoir of Campylobacter is animals especially poultry, birds, cattle, pigs and domestic pets.
- They are also found in untreated water, lakes, rivers and ponds.
- Cross-contamination occurs while handling raw meat to cooked meat and other food products and in kitchen utensils.
- Infection also occurs due to consumption of undercooked foods, raw or unpasteurized milk and milk products and raw shellfish (mainly oysters).
Disease and Complications of Campylobacteriosis
- The major cause of campylobacteriosis is gastroenteritis followed by diarrhea, inflammatory bowel disease (IBD), Barrett’s esophagus and colorectal cancer.
- The infectious dose of C. jejuni is 105cfu/ml which is capable of causing diarrhea in healthy humans.
- The signs start to appear after 1 to 3 days of ingestion with common symptoms such as watery diarrhea, malaise, fever and abdominal cramp.
- Systemic infection may also occur in severe cases like extragastrointestinal infections, lung infections, meningitis, brain abscesses, endocarditis, cellulitis and bacteremia.
- Bacteremia frequently occurs in young children and elderly patients and may lead to death.
- Some adults may show asymptomatic infection but spread the pathogens via physical contact.
- Paralysis occurs in the case of Guillain-Barre syndrome after several weeks of infection.
- Another condition develops in the knee joint and the lower back known as Reiter’s syndrome, a type of arthritis.
Epidemiology of Campylobacter Infection
- C. jejuni is the most pathogenic strain that is mostly isolated from patients suffering from diarrhea and gastrointestinal diseases.
- Campylobacteriosis cases are high in summer which might be due to the increased consumption of poultry and undercooked meat.
- The United States and England are highly affected countries during this season.
- In the US, about 8,45,000 cases of Campylobacter and 76 deaths are reported each year.
- From 2004 to 2009, the major cause of traveler’s diarrhea was associated with the Campylobacter species.
- Campylobacter has also affected the European countries with 2,14,000 cases in the year 2012 reported in the European Food Safety Authority (EFSA).
- A surveillance study was done in a multinational population with 9000 children of Bangladesh, Pakistan and India.
- The children younger than 60 months had severe diarrhea and later was detected as C. jejuni.
- C. jejuni and C. coli are more common in children and elder patients.
- People who travel abroad frequently are at high risk of C. coli infection than with C. jejuni.
- Even though the mortality rate of campylobacteriosis is less, the disease is detected every year which is due to continuous exposure to the sources like contaminated water and poultry.
Pathogenic Mechanism of Campylobacter
- Campylobacter should survive the stomach acid (pH 2.3) to cause infection however, the organism cannot survive at low pH but the infection occurs from contaminated meat, water and milk.
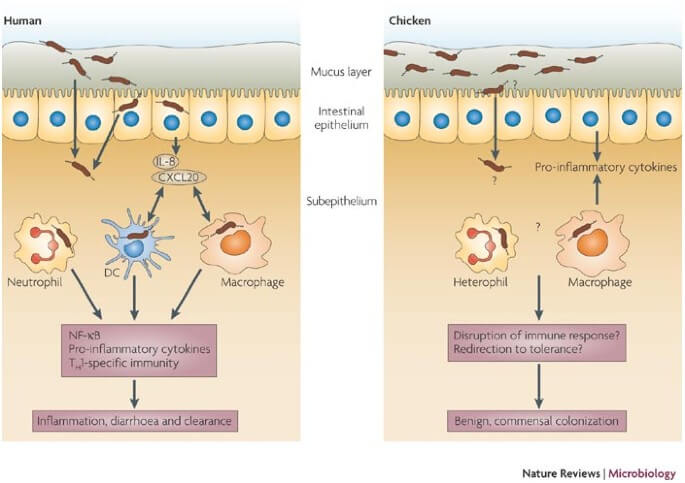
- The virulence factor and colonization of the bacteria are involved in escaping the stomach passage and reaches the gastrointestinal tract.
- Then the bacteria invade the epithelial cells of the distal ileum and colon, due to an unfavorable environment, the bacteria secrets protein that damages cells and causes inflammation of the intestinal epithelium.
- These secreted proteins are called Campylobacter virulence-associated factors which include chemotaxis, motility, flagella, cytolethal distending toxin (CDT), adhesion and invasion factors.
- The corkscrew motility of the bacteria helps in colonization and its polar flagella and chemoreceptors help to move within the mucous lining.
- Cytolethal distending toxin (CDT) is composed of three subunits namely CdtA, CdtB and CdtC each with a different mechanism.
- The CdtB subunit cleaves the enterocytes of DNA randomly that disrupts the cell wall and the death of enterocytes occur eventually.
- The CdtA and CdtC subunit binds the proteins that help CdtB to reach the enterocytes.
- Campylobacter produces adhesion proteins on its cell surface to get attached to the epithelial cells.
- Fibronectin domain-containing lipoprotein FlpA, CadF, JlpA and FlaA are the protein structure that helps in adherence of the pathogens.
- C. jejuni synthesizes four proteins namely CiaB, CiaC, CiaD and CiaI that helps in the internalization of the pathogens.
- After entering into the host cell, the pathogen multiples in a membrane-bound vacuole known as Campylobacter-containing vacuoles.
- The immune system of the human body triggers the synthesis of interleukin 8 (IL-8) that activates the T-cells and B-cells.
- The immune response of the host cell against pathogen leads to local inflammation and the Cia protein damages the tight junction resulting in diarrhea.
Diagnostic Methods of Campylobacteriosis
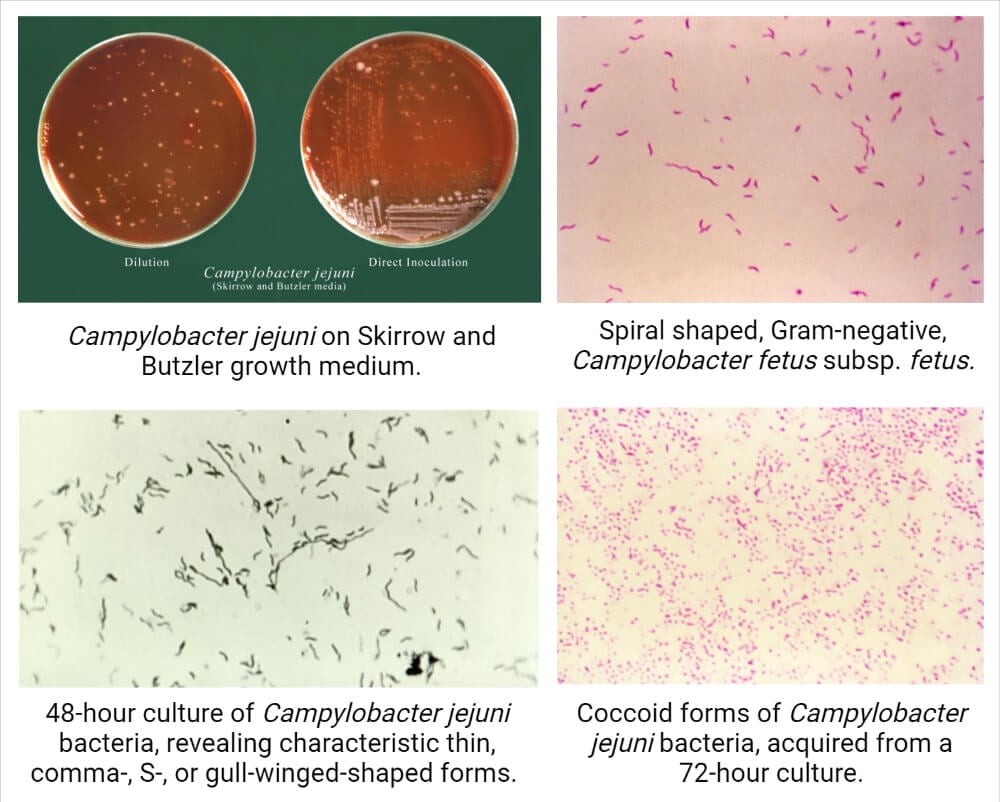
1. Culture method
- Two selective media, one blood-containing media and other charcoal-containing media are required to isolate and identify the pathogen.
- Specific antibiotics are also mixed with the media to inhibit the growth of other competitive microflora.
- Commonly used blood-containing media are sheep blood agar mixed with antibiotics such as bacitracin, colistin, cephalothin and actidione.
- Another is horse blood agar also known as the Skirrow media which includes antibiotics such as vancomycin, polymyxin B, cephalothin and trimethoprim.
- The Preston medium is the best charcoal-containing media that recover the maximum number of pathogens.
2. Molecular typing
- PCR is a widely used technique to detect the genes of most pathogens and is a highly sensitive technique but is not species-specific.
- It can detect the pathogen present in people showing no symptoms but sheds the bacteria from person to person.
- Other molecular-based typing method includes MALDI-TOF MS, multiplex PCR, Ribotyping, RFLP and AFLP.
3. Serotyping
- Heat-labile and heat-stable serotyping methods are currently used to detect Campylobacter pathogens.
- C. jejuni, C. coli and C. lari are detected by heat-labile method in which the targeted proteins are uncharacterized bacterial surface or flagella antigens.
- The heat-stable serotyping detects the heat-stable antigens from Campylobacter isolates extracted from capsular LOS. It is known as Penner serotyping.
Treatment and Control of Campylobacteriosis
- Campylobacteriosis is a self-limiting disease and the use of antibiotics is not required unless the patients have severe and bloody diarrhea.
- Erythromycin, azithromycin, gentamicin, carbapenems and chloramphenicol are the antibiotics used in C. jejuni and C. coli infections.
- In the case of gastroenteritis, erythromycin or azithromycin is used in antibiotic therapy.
- Rehydration and electrolyte therapy helps in the treatment of enteritis.
- Most of the Campylobacter species are present in poultry, the chicken with infections must be removed to reduce the environmental exposures.
- Avoid raw and unpasteurized milk, untreated water and undercooked poultry meats.
- Maintain personal hygiene during handling, producing and processing raw poultry meats which may cross-contaminate equipment and other food products.
References
- Kaakoush, N. O., Castaño-Rodríguez, N., Mitchell, H. M., & Man, S. M. (2015). Global Epidemiology of Campylobacter Infection. Clinical Microbiology Reviews, 28(3), 687–720.
- Yi, J., & Anderson, E. J. (2018). Campylobacter jejuni and Campylobacter coli. Principles and Practice of Pediatric Infectious Diseases, 899–902.e3.
- Zautner, A. E., & Masanta, W. O. (2016). Campylobacter: Health Effects and Toxicity. Encyclopedia of Food and Health, 596–601.
- Hsieh, Y.-H., & Sulaiman, I. M. (2018). Campylobacteriosis: An Emerging Infectious Foodborne Disease. Foodborne Diseases, 119–155.
- COLVILLE, J. L., & BERRYHILL, D. L. (2007). CAMPYLOBACTERIOSIS (VIBRIOSIS). Handbook of Zoonoses, 44–48.
- Oyarzabal, O. A., & Carrillo, C. D. (2017). Isolation, identification, and typing of Campylobacter strains from food samples. Campylobacter, 61–83.
- Young, K., Davis, L. & DiRita, V. Campylobacter jejuni: molecular biology and pathogenesis. Nat Rev Microbiol 5, 665–679 (2007). https://doi.org/10.1038/nrmicro1718.
- Mousavi S, Bereswill S, Heimesaat MM. Novel Clinical Campylobacter jejuni Infection Models Based on Sensitization of Mice to Lipooligosaccharide, a Major Bacterial Factor Triggering Innate Immune Responses in Human Campylobacteriosis. Microorganisms. 2020; 8(4):482. https://doi.org/10.3390/microorganisms8040482.
- Haddad N, Marce C, Magras C, Cappelier JM. An overview of methods used to clarify pathogenesis mechanisms of Campylobacter jejuni. J Food Prot. 2010 Apr;73(4):786-802. doi: 10.4315/0362-028x-73.4.786. PMID: 20377972.
- Facciolà A, Riso R, Avventuroso E, Visalli G, Delia SA, Laganà P. Campylobacter: from microbiology to prevention. J Prev Med Hyg. 2017;58(2):E79-E92.
