Interesting Science Videos
What is Chromoblastomycosis (Chromomycosis)?
Chromoblastomycosis that is also known as chromomycosis is a chronic fungal infection of the skin and the subcutaneous tissue, caused by different groups of dematiaceous fungi.
- It is one of the most encountered subcutaneous fungal infections besides sporotrichosis and mycetoma.
- Dermateciuos fungi are fungi that are pigmented, producing brown pigmentations.
- The disease is associated with slow-growing, warty plaques, cauliflower-like lesions which may ulcerate.
- It majorly affects immunocompromised individuals with a weak immune system which makes them liable to colonization and infection by these fungi.
- The fungi have a form of traumatic implantations i.e inoculation of the fungi is due to traumas such as wounds or abrasions of the skin, which exposes the skin to the fungi infection.
- The disease commonly affects male agricultural workers but few cases on children’s infections have also been documented.
Causative agents of Chromoblastomycosis (Chromomycosis)
- Chromomycosis is caused by dematiaceous fungi.
- Dermatiaceous fungi are a large group of heterogenous molds known to cause a wide range of skin infections including phaeohyphomycosis, chromoblastomycosis, and eumycotic mycetoma.
- This group of pathogenic fungi includes Fonsecaea pedrosoi, Phialophora spp, Cladophialophora bantiana, Rhinocladiella, and Exophiala spp, Mudurella spp, Scedosporium prolificans, Wangiella dermatitidis.
- The most common etiologies of chromomycosis fungi are Cladosporium carrionii, Phialophora verrucosa, and Fonsecaea pedrosoi and the least common include Fonsacea compactum, Exophiala spinifera, Rhinocladiella aquaspersa, Exophiala jeanselmei, and Wangiella dermatitidis.
- They are widely distributed in the environment, commonly found in soil, wood, and dead decaying plant debris.
- They are also common in tropical and subtropical climates.
- They contain melanin of their cell walls which determines the color of the spores.
- They reproduce asexually by forming spores known as conidia.
- They form colonies in mycological agar which are typically brown to black in color.
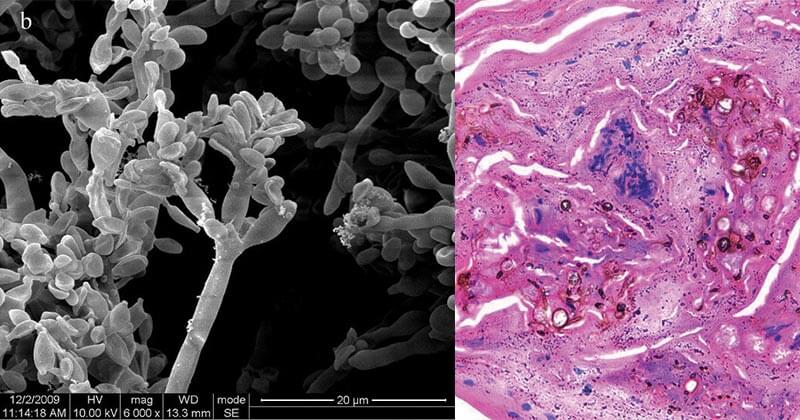
Figure: Electron micrograph of the skin showing Fonsecaea pedrosoi spores. Micrograph of chromoblastomycosis showing sclerotic bodies in the dermis. Image Source: Wikipedia.
Pathogenesis of Chromoblastomycosis (Chromomycosis)
- The fungi gain entry into the skin from trauma from vegetative materials such as thorns or splinters initiating a granulomatous response on the skin
- Mostly, the fungal infection remains asymptomatic (oligosymptomatic) for several years before it appears.
- The moderate appearance of the disease is characterized by localized pain and intensified itching which progresses to severe disease associated with edema and secondary bacterial infection which may limit body motions and activities.
- The chronic disease shows manifestations of chronic lymphoedema and development of ankylosis and non-invasive squamous cell carcinoma which may lead to patient disablement.
General manifestations will also include:
- The epidermis producing pseudoepitheliomatous hyperplasia, granuloma on the dermis associated with epithelioid cells, and Langhans giant cells.
- Fungal elements which are visualized as brown septate celled sclerotic bodies.
- Several sets of sclerotic cella include medlar bodies, muriform bodies, copper pennies.
- These bodies are extruded trans-epidermally which are seen as black dots on the surface lesions.
Risk factors of infection
- Immunocompromised patients with skin abrasions such diabetics
- Patients on medical therapies
- Wounded and surgical patients
- Agricultural workers who get skin scratching (abrasions) from plants
Virulence factors of dematiaceous fungi
- The virulence of dematiaceous fungi is associated with the presence of melanin in their cell walls, which confers a protective advantage by scavenging free radicals and hypochlorite that are produced by phagocytic cells.
- The melanin may also bind to hydrolytic enzymes, preventing the action of phagocytic cells on the plasma membrane of the fungal cells.
- The melanin gives color to the fungal spores and the fungal hyphae produced during the germination and reproduction of these fungi. This gives the fungi a pigmentation that produces colored skin lesions and skin manifestations.
Clinical Features of Chromoblastomycosis (Chromomycosis)
Chromoblastomycosis is presented with:
- Small firm red or grey bump.
- The bump grows slowly about 2mm per year.
- A dr warty nodule or plaque develops with centered scarring.
- The affected limb enlarges causing elephantiasis
- The scarred lesion then forms new lesions around the scar allowing spread to new sites with itchiness.
- Squamous cell carcinoma may develop due to longterm infection of chromoblastomycosis.
The lesions developed during chromoblastomycosis infections include:
- Nodular lesions are moderately elevated, fairly soft, with a dull to pink violaceous growth with a smooth surface, verrucous, or scaly. They gradually become tumorous with time.
- Tumoral lesions are tumor-like masses, prominent, papillomatous, sometimes lobulated; ‘cauliflower-like’; covering the surface partially or entirely with epidermal debris and crusts. they are more exuberant and occurs majorly in lower extremities.
- Cicatricial lesions are non-elevated with an enlarged peripheral extension and atrophic scarring. They have centered healing. They have an annular, arciform, or serpiginous outline and they can occur extensively in parts of the body.
- Plaques are slightly elevated lesions occurring in various sizes and shapes with infiltration. They are reddish to violaceous in color with a scaly surface and may have marked lines of cleavage. They are generally found on the higher parts on the limbs.
- Verracuous are outwardly hyperkeratosis lesions that are warty dry and are commonly found along the border of the foot.
Diagnosis of Chromoblastomycosis (Chromomycosis)
Clinical Diagnosis
Clinical observation of lesions and differentiation from other characteristic lesions formed by other microbial agents and fungal agents as described above.
Laboratory Diagnosis
Specimen: Lesion exudates, skin scrapings, crusts, aspirated debris, and tissue fragments
Direct examination and microscopy
- 20-40% KOH wet mount to observe muriform (single or clustered) cells in clinical samples which are 5 to 12 µm in diameter, round to polyhedral (chestnut) in shape, thick-walled, dark pigmented, and having both transverse and longitudinal cross-walls resembling a brick wall.
- Hematoxylin-eosin staining for tissue samples for observation of the muriform cells.
- Calcofluor white dye stain
Cultural Examination
- Use of mycological and bacterial cultures to isolate pigmented fungal spores which are examined by KOH wet mount for identification of muriform cells.
- However, cultural methods are inadequate and unconventional therefore require to follow up examination using staining and microscopic techniques.
Histological Examination
- Tissue samples and biopsies for the identification of lesion particles such as granulomatous tissue elements, and giant cells from lesions.
Molecular Identification of agents
- Duplex PCR targeting the ribosomal DNA for Fonsecaea spp., and a specific oligonucleotide primer for identification of C. carrionii
Immunological Examination
- This can be used to identify the production of antibodies against the fungal antigens such as ELISA assay using C. carrionii antigen AgSPP.
Treatment of Chromoblastomycosis (Chromomycosis)
- Treatment for Chromoblastomycosis includes physical therapeutic methods as well as topical and systemic therapy with antifungal agents, which have been documented to be effective.
- Physical Therapeutics includes surgery, thermotherapy, laser therapy, and photodynamic therapy (PDT) along with combined therapies of antifungal drugs.
- Use of antifungal agents such as itraconazole(ITZ), voriconazole (VCZ), PCZ, and isavuconazole (ISA). Itraconazole is used as the first line of treatment for CBM and Terbinafine is the second most frequently used antifungal agent for the treatment of CBM.
- Combination therapy with systemic antifungal drugs has been used in the salvage therapy scenario for patients with invasive refractory mycoses such as a combination of itraconazole with terbinafine.
- Combined therapy may also include the use of antifungal agents along with physical therapeutics such as surgeries.
- Adjuvant therapy has also been used as a form of treatment which includes the use of antifungal drugs with immunomodulant adjuvants in severe and refractory cases of infection. Adjuvants such as Imiquimod, (1→3)-β-polyglucoside have been used with itraconazole and terbinafine antifungals.
- BM treatment must be monitored by clinical, mycological, and histopathological criteria to ensure clearance of lesions and scars for conclusively complete healing of the disease.
Antifungal Resistance of causative agents of chromoblastomycosis
- Chromoblastomycosis is a chronic fungal infection that has shown resistance to normal antifungal therapies such as fluconazole and amphotericin B, and therefore the use of broad-spectrum therapies such as itraconazole and terbinafine are used.
Prevention and Control of chromoblastomycosis
- Due to a lack of vaccines specific for chromoblastomycosis, it advised that the use of protective clothing such as gloves, shoes, and clothes to reduce the risk of infection by ubiquitously dematiaceous fungi, especially to the occupationally risky groups.
References
- Epidemiology, Clinical Manifestations, and Therapy of Infections Caused by Dematiaceous Fungi by M.E Brandt and Warnock D. W. PubMed.gov
- Chromoblastomycosis (Chromomycosis) by George Kurien; Kavin Sugumar; Veena Chandran. NCBI
- Exophiala psychrophila: A new agent of chromoblastomycosis by Lina M. Garzon, Lili J. Rueda, Adriana Marcela Celis, Martha Cardena, and Marcela Guevara-Suarez. NCBI
- Agents of Chromoblastomycosis by Duane R. Hospenthal. ScienceDirect
- Dematiaceous fungi by Deanna A. Sutton, Michael G. Rinaldi, Stephen E. Sanche. ScienceDirect
- Chromoblastomycosis: an overview of clinical manifestations, diagnosis, and treatment by
- Chromoblastomycosis by , , , , , , , , , , , ,
Sources
- 1% – https://www.woundsinternational.com/uploads/resources/content_10454.pdf
- 1% – https://www.sciencedirect.com/topics/nursing-and-health-professions/chromomycosis
- 1% – https://www.researchgate.net/publication/257779133_Chromoblastomycosis_in_the_Clinical_Practice
- 1% – https://www.ncbi.nlm.nih.gov/pubmed/15207119
- 1% – https://www.dermnetnz.org/topics/chromoblastomycosis/
- 1% – https://www.deepdyve.com/lp/wiley/dematiaceous-fungi-AEm88tQ54y
- 1% – http://www.differencebetween.net/science/health/drugs-health/difference-between-itraconazole-and-terbinafine/
- <1% – https://www.nrcresearchpress.com/doi/abs/10.1139/m97-021
- <1% – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5087237/
- <1% – https://www.antiinfectivemeds.com/fungal-infections/chromomycosis/
- <1% – https://pubchem.ncbi.nlm.nih.gov/compound/itraconazole
- <1% – https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1469-185X.1984.tb00404.x
- <1% – https://medicalyrelated.blogspot.com/2015/05/mycology.html

Thank you for helping